You only have one more appointment to go until lunch, and you’re hoping it’ll be an easy one. You’re more than ready to sit down, enjoy your sandwich, and take a well-deserved break.
But no such luck. Waiting in the exam room is Ralphie, an 8-year-old male domestic longhair who hasn’t been acting like himself for the past week. When you enter the exam room, you greet his owner, Gemma, and then take a peek into his carrier. You immediately notice he is tachypneic and occasionally open-mouth breathing.
You’re instantly concerned. You know that if you get Ralphie out of his carrier and perform a physical exam, his condition may quickly go from bad to worse.
But you also know you need to figure out what is going on with Ralphie as soon as possible so you can get started on treatment. It’s a fine balance to strike.
But with the support of the veterinary algorithms in Plumb’s Pro™, you’ve got this.
Step 1: Start With Stabilization and History-Taking
You explain to Gemma that Ralphie appears to be in respiratory distress, and it’s important to try to stabilize his condition before proceeding.
You place Ralphie in an oxygen cage and instruct your technician to monitor him closely before heading back into the exam room to get more details from Gemma.
She says that while Ralphie is normally a very social and affectionate cat, he’s been spending a lot of time hiding under the bed recently. His appetite has been lower over the past week, and Gemma isn’t sure if he ate anything at all yesterday. She noticed him breathing more quickly than usual last night but hadn’t seen him coughing or sneezing.
Ralphie had been doing fairly well until now. He generally has a sensitive stomach and vomits about every other day. Gemma had recently switched him to a hairball formula diet to see if that would help, but last week he vomited several times in one day. He is indoor-only and the only pet in the home. He is up to date on vaccinations and not on any medications or parasite preventives.
Armed with this information, you head back into the treatment area to see how Ralphie is doing and decide on your next steps.
Step 2: Perform a Physical Exam While Minimizing Stress
Ralphie appears fairly comfortable in the oxygen cage, and his respiratory rate on distant exam is 52 breaths per minute. He is no longer open-mouth breathing.
You decide to remove Ralphie from the cage to perform a brief physical exam. His mucous membranes appear slightly pale, and his heart rate is 200 bpm with no murmur or arrhythmia auscultated. His lung sounds are increased with crackles on the right side. His weight is 4.2 kg with a body condition score of 4/9 and his temperature is slightly low at 98°F. No abnormalities are found on abdominal palpation. His SpO2 is 95%.
You place Ralphie back in the oxygen cage while you decide on your differentials and next steps.
Looking for more support tackling respiratory distress? Download a free, step-by-step guide to stabilizing these patients.
Step 3: Turn to an Algorithm for Step-by-Step Support
You need to get rolling on diagnostics so you can choose the treatments that will help Ralphie breathe more easily, but any amount of handling and stress could tip him over the edge. It’s crucial to come up with a game plan that allows you to be as efficient as possible.
That’s where algorithms come in. These visual clinical roadmaps are designed to use the information you have—like clinical signs or diagnostic results—to help you swiftly narrow down your differentials and decide on the next steps.
You grab your phone and open Plumb’s Pro™. You search for respiratory disease and find an algorithm for localizing the anatomic site of respiratory disease.
Ralphie’s dominant clinical sign is his abnormal breathing pattern, so you follow the algorithm for tachypnea, and it suggests you start with thoracic radiography and thoracic point-of-care ultrasound.
Before performing diagnostics, you want to ensure Ralphie is as stable and relaxed as possible. You elect to give him an intramuscular injection of butorphanol (0.2 mg/kg) to help reduce his anxiety, along with a single injection of furosemide (2 mg/kg IM), in case he has pulmonary edema secondary to cardiac disease.
After 15 minutes, Ralphie seems more relaxed and his respiratory rate has decreased a little (46 bpm). Unfortunately, your colleague with experience performing thoracic point-of-care ultrasound procedures isn’t in the clinic today, so you elect to proceed with thoracic radiography.
You find a moderate interstitial to alveolar pulmonary pattern in the cranioventral lung fields, primarily involving the right middle lung lobe. You can’t appreciate any obvious masses or pleural effusion on the radiographs, and Ralphie’s heart appears normal in size and shape.
You return to the algorithm and look at the differentials listed under “interstitial to alveolar pattern.”
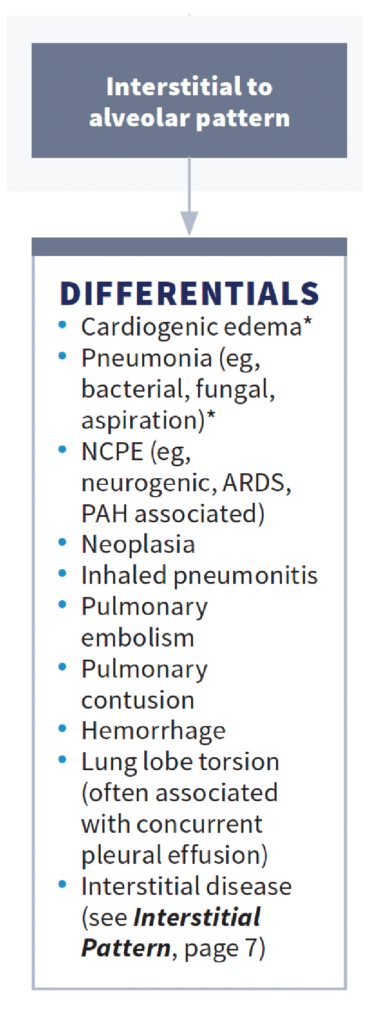
Based on the radiographic findings and Ralphie’s history of chronic vomiting, your primary differential is aspiration pneumonia. But you’d like to perform blood work to help confirm this and rule out other differentials, and Gemma agrees to proceed.
Step 4: Connect the Dots With Baseline Diagnostics
You obtain a blood sample from Ralphie and place him back in the oxygen cage while waiting for the results. You run an in-clinic CBC and serum chemistry profile and perform point-of-care testing for retroviruses and N‐terminal pro–B‐type natriuretic peptide (NT‐proBNP).
The CBC reveals moderate neutrophilia with a left shift, consistent with infection or inflammation. No abnormalities are present on his chemistry profile aside from mild stress hyperglycemia. The results of his NT-proBNP test are normal, and his retroviral testing is negative.
Based on these findings, Ralphie’s radiographs, and his history of chronic vomiting, you are suspicious of aspiration pneumonia. You discuss your suspicions with Gemma and suggest a bronchoalveolar lavage to confirm bacterial pneumonia. She declines due to financial constraints and elects to proceed with treatment for presumed aspiration pneumonia.
Step 5: Make a Treatment Plan and Share Client Handouts
You return to Plumb’s Pro™ and consult the Dx & Tx on aspiration pneumonia for accurate, peer-reviewed treatment guidelines.

You plan to hospitalize Ralphie for 48-72 hours and start him on cefazolin (25 mg/kg IV slowly every 6 hours), along with IV fluids to maintain hydration and oxygen supplementation as needed. You discuss with Gemma that Ralphie will be on antibiotics for at least 14 days, but it may be much longer based on how Ralphie is doing on follow-up exams and thoracic radiographs.
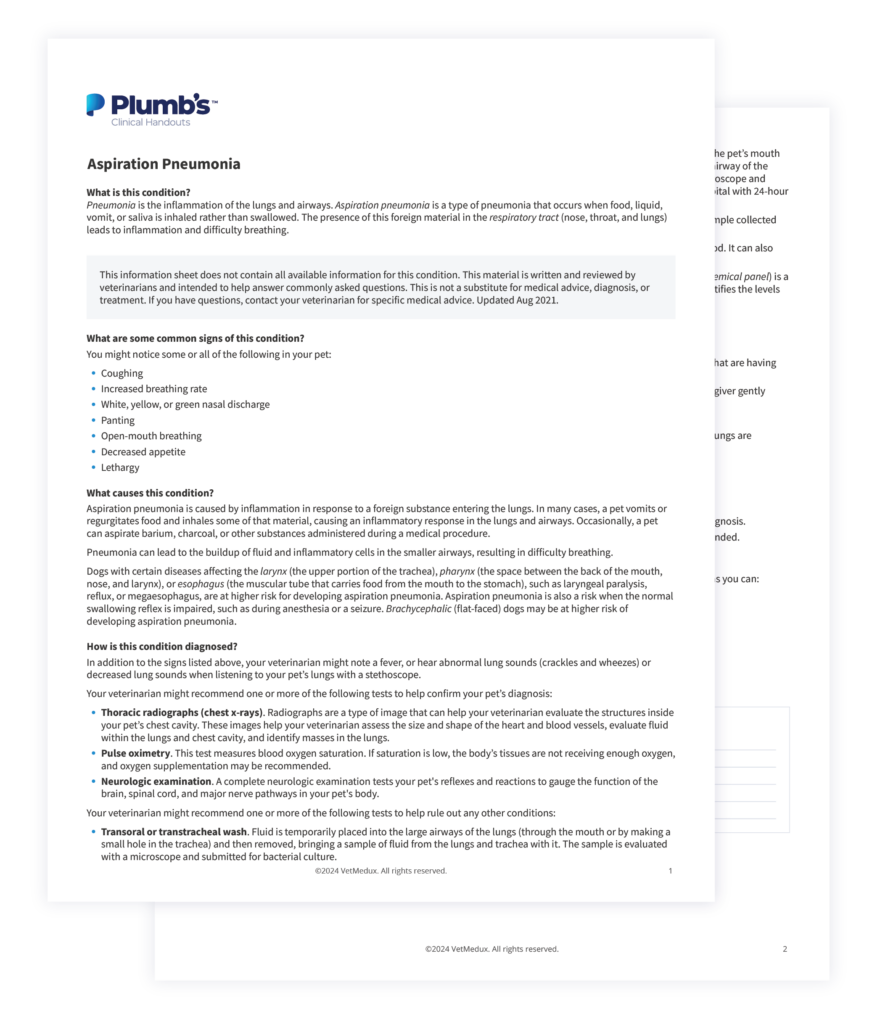
You send Gemma home with the Plumb’s™ client handout on aspiration pneumonia, and you explain that further workup for Ralphie’s chronic vomiting will be needed in the future and will be discussed at his follow-up visit.
How to Chart a Clear Path Forward with Algorithms
Ralphie’s case demonstrates how algorithms can help you narrow down your differentials, ensure you don’t miss any steps along the way, and guide client communication.
They’re helpful in emergency situations, particularly when the adrenaline rush makes it difficult to think clearly. But they can also help you double-check your thinking during routine cases to ensure you’re not missing anything, walk you through complex cases, and help you regroup when your patient isn’t responding to treatment as expected.
You can find algorithms in Plumb’s Pro™ with a quick search by clinical condition, test result, or diagnosis. Once you click the title, the algorithm will open right within the app or website for easy navigation.

The algorithms in Plumb’s Pro™ are the ideal decision-making tool and are just one of the essential practice tools included in Plumb’s Pro™.


